Pneumomediastinum in the COVID-19 era: to drain or not to drain?
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Accepted: 20 July 2022
Authors
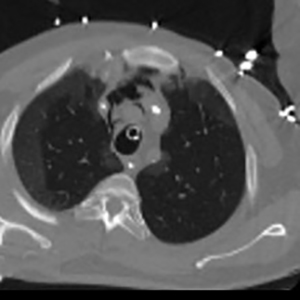
Pneumomediastinum (PNM) is a rare clinical finding, usually with a benign course, which is managed conservatively in the majority of cases. However, during the COVID-19 pandemic, an increased incidence of PNM has been observed. Several reports of PNM cases in COVID-19 have been reported in the literature and were managed either conservatively or surgically. In this study, we present our institutional experience of COVID-19 associated PNM, propose a management algorithm, and review the current literature. In total, 43 Case Series were identified, including a total of 747 patients, of whom 374/747 (50.1%) were intubated at the time of diagnosis, 168/747 (22.5%) underwent surgical drain insertion at admission, 562/747 (75.2%) received conservative treatment (observation or mechanical ventilation. Inpatient mortality was 51.8% (387/747), while 45.1% of the population recovered and/or was discharged (337/747). In conclusion, with increased incidence of PNM in COVID-19 patients reported in the literature, it is still difficult to assign a true causal relationship between PNM and mortality. We can, however, see that PMN plays an important role in disease prognosis. Due to increased complexity, high mortality, and associated complications, conservative management may not be sufficient, and a surgical approach is needed.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






