Varicella zoster virus and cardiovascular diseases
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
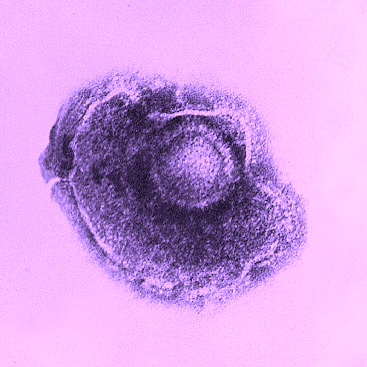
Varicella zoster virus (VZV) is a Herpesviridae family double-stranded DNA virus that only affects humans. The first clinical manifestation appears to be varicella, typical of childhood. VZV, on the other hand, becomes latent in ganglion neurons throughout the neuroaxis after primary infection. The VZV reactivates and travels along peripheral nerve fibers in the elderly and immunocompromised individuals, resulting in Zoster. It can, however, spread centrally and infect cerebral and extracranial arteries, resulting in vasculopathy, which can lead to transient ischemic attacks, strokes, aneurysms, cavernous sinus thrombosis, giant cell arteritis, and granulomatous aortitis. Although the mechanisms of virus-induced pathological vascular remodeling are not fully understood, recent research indicates that inflammation and dysregulation of ligand-1 programmed death play a significant role. Few studies, on the other hand, have looked into the role of VZV in cardiovascular disease. As a result, the purpose of this review is to examine the relationship between VZV and cardiovascular disease, the efficacy of the vaccine as a protective mechanism, and the target population of heart disease patients who could benefit from vaccination.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






