Detection of clinically-relevant EGFR variations in de novo small cell lung carcinoma by droplet digital PCR
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
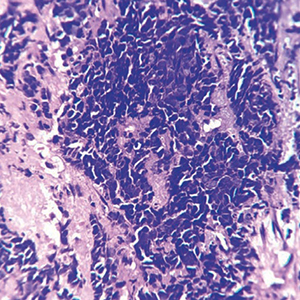
Targeted therapy that utilizes tyrosine kinase inhibitors (TKIs), specific to epidermal growth factor receptors (EGFR) has changed the landscape of treatment of non-small cell lung cancer (NSCLC). The success or failure of this approach depends on presence of certain variations in the tyrosine kinase domain of EGFR gene. Generally, patients diagnosed with Small cell lung cancer (SCLC) are considered ineligible for TKI therapy owing to the absence of EGFR variations. . However, there is evidence of these variations being detected in SCLCs, both in de-novo and in transformed SCLCs (TKI-treated adenocarcinomas). Despite the presence of clinically-relevant EGFR variations in SCLCs, the response to TKIs has been inconsistent. Liquid biopsy is a well-established approach in lung cancer management with proven diagnostic, prognostic and predictive applications. It relies on detection of circulating tumor-derived nucleic acids present in plasma of the patient. In this study, a liquid biopsy approach was utilized to screen 118 consecutive lung cancer patients for four clinically-relevant variations in EGFR gene, which included three activating/sensitizing variations (Ex18 G719S, Ex19del E746-A750 and Ex21 L858R) and one acquired/resistance (Ex20 T790M, de novo) variation by droplet digital PCR, the most advanced third generation PCR technique. As expected, clinically-relevant EGFR variations were found in majority of the non-small cell lung cancer cases. However, among the handful of small cell lung cancer samples screened, sensitizing variations (Ex18 G719S and Ex21 L858R) were seen in almost all of them. Interestingly, Ex20 T790M variation was not detected in any of the cases screened. The results of our study indicate that EGFR variations are present in SCLCs and highly sensitive liquid biopsy techniques like ddPCR can be effectively utilized for this purpose of screening EGFR variations in such samples.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






