Cardiology - Case Reports
Vol. 93 No. 4 (2023)
Serratia endocarditis, uncommon organism, with significant complications
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Received: 8 October 2022
Accepted: 13 January 2023
Accepted: 13 January 2023
1380
Views
366
Downloads
Authors
Department of Internal Medicine, Saint Vincent Hospital, Worcester, MA, United States.
Department of Internal Medicine, Saint Vincent Hospital, Worcester, MA, United States.
Department of Clinical Cardiology, Saint Vincent Hospital, Worcester, MA, United States.
Department of Clinical Cardiology, Saint Vincent Hospital, Worcester, MA, United States.
Department of Clinical Cardiology, Saint Vincent Hospital, Worcester, MA, United States.
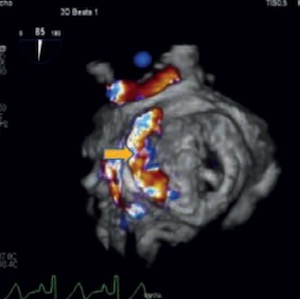
Serratia marcescens is an aerobic, Gram-negative bacillus predominantly seen in patients with intravenous drug use, immunosuppression, previous antibiotic exposure, and indwelling catheterization. Gram-negative organism causing infective endocarditis (IE) is rare. Serratia marcescens IE is uncommon and is reported to be seen in 0.14% of all cases. In this report, we discuss in detail about a 38-year-old man with a history of intravenous drug abuse presenting with S. marcescens related prosthetic valve IE.
Richardson A, Martinez A, Ghetiya S, et al. Serratia marcescens endocarditis with perivalvular abscess presenting as atrioventricular block. Case Rep Infect Dis 2020;2020:7463719. DOI: https://doi.org/10.1155/2020/7463719
Yeung H-M, Chavarria B, Shahsavari D. A complicated case of Serratia marcescens infective endocarditis in the era of the current opioid epidemic. Case Rep Infect Dis 2018;2018:5903589. DOI: https://doi.org/10.1155/2018/5903589
Mishra AK, Sahu KK, Lal A, Menon V. Aortic valve abscess: Staphylococcus epidermidis and infective endocarditis. QJM 2020;113:211-2. DOI: https://doi.org/10.1093/qjmed/hcz151
Sahu KK, Mishra AK, Sherif AA et al. An interesting case of pacemaker endocarditis. Neth Heart J 2019;27:585-6. DOI: https://doi.org/10.1007/s12471-019-01310-2
Mishra AK, Sahu KK, Lal A. Significance of prolonged PR interval in infections. QJM 2020;113:150-1. DOI: https://doi.org/10.1093/qjmed/hcz192
Hadano Y, Kamiya T, Uenishi N. A fatal case of infective endocarditis caused by an unusual suspect: Serratia marcescens. Intern Med 2012;51:1425-8. DOI: https://doi.org/10.2169/internalmedicine.51.6648
Mishra AK, Sahu KK, Lal A, Sujata M. Systemic embolization following fungal infective endocarditis. QJM 2020;113:233-5. DOI: https://doi.org/10.1093/qjmed/hcz274
Sahu KK, Mishra AK, Lal A, Kranis M. An interesting case of expressive aphasia: Enterococcus faecalis-related infective endocarditis complicating as septic emboli. QJM 2020;113:146-7. DOI: https://doi.org/10.1093/qjmed/hcz169
Mishra A, Sahu K, Nagabandi S, Benotti J. Infective endocarditis with mitral leaflet perforation and multiple embolic infarcts. QJM 2020;113:757-9. DOI: https://doi.org/10.1093/qjmed/hcaa026
Thomas VV, Mishra AK, Jasmine S, Sathyendra S. Gram-negative infective endocarditis: a retrospective analysis of 10 years data on clinical spectrum, risk factor and outcome. Monaldi Arch Chest Dis 2020;90:1359. DOI: https://doi.org/10.4081/monaldi.2020.1359
Mishra A, Sahu KK, Abraham BM, et al. Predictors, patterns and outcomes following Infective endocarditis and stroke. Acta Biomed 2022;93:e2022203.
Bakhit A, Mishra AK, Choudhary K, Khaled Soufi M. Aortic root fistula complicating Austrian syndrome. Monaldi Arch Chest Dis 2021;91:1834. DOI: https://doi.org/10.4081/monaldi.2021.1834
Mishra AK, Sahu KK, George AA, Lal A. Safety and efficacy of thrombolysis and mechanical thrombectomy in infective endocarditis. J Stroke Cerebrovasc Dis 2020;29:104784. DOI: https://doi.org/10.1016/j.jstrokecerebrovasdis.2020.104784
Phadke VK, Jacob JT. Marvelous but morbid: infective endocarditis due to Serratia marcescens. Infect Dis Clin Pract (Baltim Md) 2016;24:143-50. DOI: https://doi.org/10.1097/IPC.0000000000000360
Mishra AK, Sahu KK, Baddam V, Sargent J. Stroke and infective endocarditis. QJM 2020;113:515-6. DOI: https://doi.org/10.1093/qjmed/hcaa098
Mishra AK, Lal A, George AA. Letter by Mishra et al Regarding Article, "Infection as a stroke trigger: Associations between different organ system infection admissions and stroke subtypes". Stroke 2019;50:e328. DOI: https://doi.org/10.1161/STROKEAHA.119.026990
Dahl A, Hernandez-Meneses M, Perissinotti A, et al. Echocardiography and FDG-PET/CT scan in Gram-negative bacteremia and cardiovascular infections. Curr Opin Infect Dis 2021;34:728-36. DOI: https://doi.org/10.1097/QCO.0000000000000781
Mishra AK, Abraham BM, Sahu KK, et al. Harms and contributors of leaving against medical advice in patients with infective endocarditis. J Patient Saf 2022;18:756-9. DOI: https://doi.org/10.1097/PTS.0000000000001055
George A, Alampoondi Venkataramanan SV, John KJ, Mishra AK. Infective endocarditis and COVID -19 coinfection: An updated review. Acta Biomed 2022;93:e2022030.
Ioannou P, Alexakis K, Spentzouri D, Kofteridis DP. Infective endocarditis by Serratia species: a systematic review. J Chemother 2022;34:347-59. DOI: https://doi.org/10.1080/1120009X.2022.2043513
How to Cite
“Serratia Endocarditis, Uncommon Organism, With Significant Complications”. 2023. Monaldi Archives for Chest Disease 93 (4). https://doi.org/10.4081/monaldi.2023.2453.
Copyright (c) 2023 The Author(s)


This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






