Oxygen-induced hypercapnia: physiological mechanisms and clinical implications
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
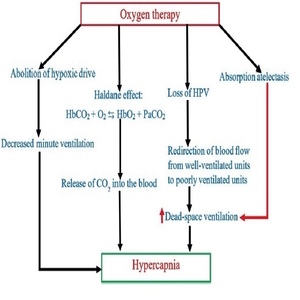
Oxygen is probably the most commonly prescribed drug in the emergency setting and is a life-saving modality as well. However, like any other drug, oxygen therapy may also lead to various adverse effects. Patients with chronic obstructive pulmonary disease (COPD) may develop hypercapnia during supplemental oxygen therapy, particularly if uncontrolled. The risk of hypercapnia is not restricted to COPD only; it has also been reported in patients with morbid obesity, asthma, cystic fibrosis, chest wall skeletal deformities, bronchiectasis, chest wall deformities, or neuromuscular disorders. However, the risk of hypercapnia should not be a deterrent to oxygen therapy in hypoxemic patients with chronic lung diseases, as hypoxemia may lead to life-threatening cardiovascular complications. Various mechanisms leading to the development of oxygen-induced hypercapnia are the abolition of ‘hypoxic drive’, loss of hypoxic vasoconstriction and absorption atelectasis leading to an increase in dead-space ventilation and Haldane effect. The international guideline recommends a target oxygen saturation of 88% to 92% in patients with acute exacerbations of chronic obstructive pulmonary disease (AECOPD) and other chronic lung diseases at risk of hypercapnia. Oxygen should be administered only when oxygen saturation is below 88%. We searched PubMed, EMBASE, and the CINAHL from inception to June 2022. We used the following search terms: “Hypercapnia”, “Oxygen therapy in COPD”, “Oxygen-associated hypercapnia”, “oxygen therapy”, and “Hypoxic drive”. All types of study are selected. This review will focus on the physiological mechanisms of oxygen-induced hypercapnia and its clinical implications.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






