Pulmonary rehabilitation: A novel adjunct in management of obstructive sleep apnea
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
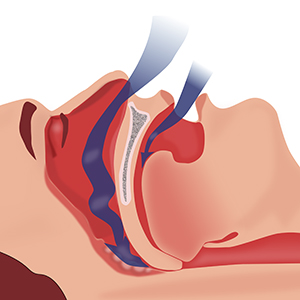
Pulmonary rehabilitation (PR) is being used in the routine management of patients of obstructive sleep apnea (OSA) at some centers. However, the studies documenting benefits of PR in OSA lack standardization in terms of outcome measures. A study was hence planned to determine the efficacy of PR on exercise capacity, health related quality of life (HRQOL), day time sleepiness and sleep-quality of life (QOL) in patients of OSA. As a part of comprehensive therapy, patients diagnosed with OSA are managed with continuous positive airway pressure (CPAP), 8 weeks thrice weekly outpatient hospital-based PR and medical treatment at the Pulmonary Medicine Department, Government Medical College and Hospital, Chandigarh. However, some patients refuse for PR because of time constraints and travel issues. Patients with newly diagnosed OSA without co-existing respiratory disease, who agreed for the CPAP, PR and medical management were enrolled in group A. The patients who refused for PR but were ready for CPAP and medical management were enrolled in Group B; 30 patients were taken in each group. Exercise capacity, HRQOL, day time sleepiness and sleep-QOL were determined at baseline and at 8-weeks follow-up by 6-minute walk distance (6MWD), St. George's Respiratory Questionnaire (SGRQ), Epworth Sleepiness Scale (ESS) and Functional Outcomes of Sleep Questionnaire (FOSQ) and compared amongst the two groups. Four patients from group A were excluded as they did not complete PR; 26 patients from group A and 30 patients from group B were finally analyzed. At baseline, both groups were matched with respect to age, gender, apnea-hypopnea index (AHI), body mass index (BMI), FEV1%predicted, 6MWD, SGRQ, ESS and FOSQ. At follow up at 8 weeks, BMI, 6MWD, SGRQ, ESS and FOSQ improved significantly from baseline in group A (p<0.001). FEV1%predicted also improved but non significantly. In group B, FEV1%predicted, BMI, 6MWD, SGRQ, ESS and FOSQ score did not improve significantly from baseline. Mean improvement from baseline in BMI, 6MWD, SGRQ, ESS and FOSQ was significantly more in group A than group B (p<0.001, p<0.001, p=0.041, p<0.001 and p<0.001, respectively). PR, being beneficial, should be incorporated in standard management of OSA.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






