Use of flow volume curve to evaluate large airway obstruction
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
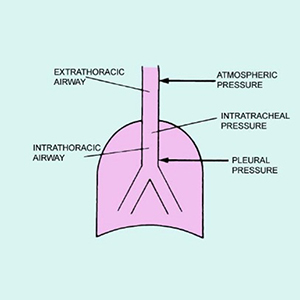
The flow volume loop (FVL) is a graphic display of airflow against lung volumes at different levels obtained during the maximum inspiratory and expiratory maneuver. It is a simple and reproducible method of lung function assessment. A narrative review was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines. PubMed, EMBASE, Ovid MEDLINE and CINAHL databases were queried and reviewed for studies pertinent to the various FVLs abnormalities and their mechanisms from January 2020 to December 2020. We used the following search terms; flow-volume loop, upper airway obstruction, Obstructive airway disease, and spirometry. Assessing the shape of the flow-volume loop is particularly helpful in diagnosing and localizing upper airway obstruction. They are also helpful in identifying bronchodilator response to treatment. Characteristic FVLs is also seen in patients with obstructive or restrictive lung disorders. Spirometry should be interpreted using the absolute values for flows and volumes as well as the flow volume and volume time curves.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






