Role of esophageal manometry in polysomnography of patients with chronic respiratory failure
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
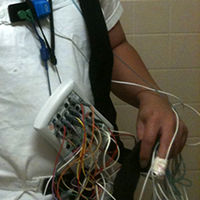
Esophageal pressure (Pes) monitoring is performed during polysomnography (PSG) with a thin, water-filled catheter connected to a transducer. The resulting quantitative assessment of respiratory effort can aid in the accurate diagnosis of sleep-related breathing disorders. This was a prospective observational study using Pes in PSG for thirty patients with chronic respiratory failure (CRF) conducted in the Department of Pulmonary, Critical Care and Sleep Medicine at a tertiary care centre of North India. Sleep scoring was done by conventional method and using esophageal manometry and compared polysomnography normal without esophageal manometry recording (PSGN) and polysomnography with esophageal manometry scoring (PSGE). Apnea hypopnea index (AHI) index was similar in both groups. However, respiratory effort related arousals (RERAs) were diagnosed easily using Pes resulting in significant increase in respiratory disturbance index (RDI) and even reclassification in terms of severity of sleep apnea. Besides, Pes was also useful to distinguish obstructive from central hypopnea which cannot be distinguished by routine PSG which can help guide therapy particularly in chronic respiratory failure patients with hypoventilation. Such patients with hypoventilation often require bilevel positive airway pressure as ventilatory support. Central hypopneas and apneas with hypercapnia may require higher-pressure support, a backup rate or even advanced volume assured modes of ventilation. Thus, it can be concluded that Pes in PSG remains a safe and generally well-tolerated procedure. Use of Pes aids to detect RERA and thereby RDI; a better marker of sleep-related breathing disorder rather than AHI. It also helps in differentiating between obstructive and central hypopnea.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






