Lung ultrasound: a narrative review and proposed protocol for patients admitted to Cardiac Rehabilitation Unit
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Accepted: 26 June 2021
Authors
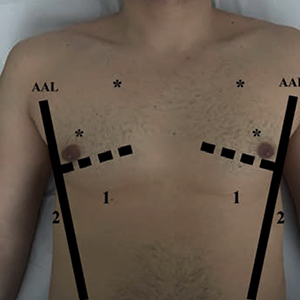
Lung ultrasonography (LUS) has become in the last 10 years a technique that has reduced the need of second level diagnostic methods such as chest X-ray (CXR) and computerize tomography (CT) for the diagnostic imaging of lung and pleural space, throughout its diagnostic accuracy, radiation free, low cost, real time and bedside approach. The common use of LUS has been recently extend to cardiac and pulmonary disease even in context of Cardiac Rehabilitation Unit and it could be an additional tool for physiotherapist for the management of patients during Rehabilitation course. The authors performed a literature review in PubMed and suggested a new standardize protocol for LUS, based on guidelines and expert consensus document, for patients admitted to Cardiac Rehabilitation Unit. In this protocol, LUS should be performed in six scan each hemithorax, covering twelve imagine regions. For each scan will be noted a specific physiologic or pathological patterns. Furthermore, we suggest for each patient, the use of the Lung Ultrasound Score (LUS score) to obtain a global view of lung aeration and to monitor any changes during the hospitalization. An increase in score range indicates a more severe condition. This Lung Ultrasonography Protocol should be performed in all patients at the time of admission to Cardiac Rehabilitation Unit to monitoring the aeration of the lungs and the possible lung and/or pleura complications after a cardiac disease avoiding the use of second level surveys.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






