Comparative analysis of airway invasive aspergillosis and endobronchial spread of tuberculosis on high resolution computed tomography
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Accepted: 18 October 2022
Authors
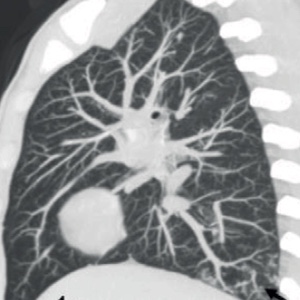
The presence of tree-in-bud (T-I-B) pulmonary opacities on high resolution computed tomography (HRCT) in tuberculosis endemic areas is frequently regarded as a sine qua non for endobronchial tuberculosis (TB). That is not always the case, however. They can also be found in immunocompromised non-neutropenic patients with airway invasive aspergillosis (IA). Understanding the differences between the two conditions is thus critical for making an accurate diagnosis. This research aims to pinpoint those distinguishing characteristics. The study defines the distribution and morphology of T-I-B opacities and other ancillary pulmonary findings in the two conditions by performing a retrospective analysis of HRCT features in 53 immunocompromised patients with lower respiratory tract symptoms, 38 of whom were positive for TB on BAL fluid analysis and 15 confirmed IA by Galactomannan method. While the global distribution of T-I-B opacities affecting all lobes favoured TB (p=0.002), the basal distribution overwhelmingly favoured IA (p<0.0001). Morphologically, dense nodules with discrete margins were associated with TB, whereas nodules with ground-glass density and fuzzy margins were associated with IA. Clustering of nodules was observed in 18 TB patients (p=0.0008). Cavitation was found in 14 (36.84%) of TB patients but not in any of the IA patients. Peri-bronchial consolidation was found in seven (46.67%) of the IA cases and four (10.53%) of the TB cases (p=0.005, 0.007). The presence of ground-glass opacity and bronchiectasis did not differ significantly between the two groups. Not all T-I-B opacities on HRCT chest in immunocompromised patients in endemic TB areas should be reported as tubercular. Immunocompromised non-neutropenic patients with airway IA can be identified earlier with tree-in-bud opacities on HRCT chest, even in the absence of a nodule with halo, resulting in earlier and more effective management.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






