Homocysteine and atrial fibrillation: novel evidences and insights
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Accepted: 9 April 2022
Authors
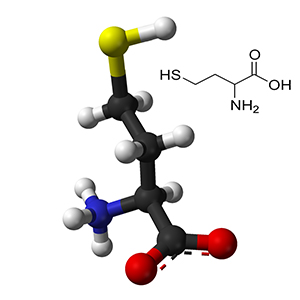
Atrial fibrillation (AF) is one of the most prevalent rhythm disorders worldwide, with around 37.574 million cases around the globe (0.51 % global population). Different studies showed a high informative value of different biomarkers, including such related to the systemic inflammation, biomechanical stress and fibrosis. In this review article we aimed to study only the relation of homocysteine to the AF development. Homocysteine is a sulfur-containing amino acid, that is produced in the process of methionine metabolism. Which is a non-canonical amino acid, that is derived from the food proteins. From the scientific point of view there is a relation between hyperhomocysteinemia and myocardial fibrosis, but these mechanisms are complicated and not sufficiently studied. Homocysteine regulates activity of the ion channels through their redox state. Elevated homocysteine level can condition electrical remodeling of the cardiomyocytes through the increase of sodium current and change in the function of rapid sodium channels, increase of inwards potassium current and decrease in amount of rapid potassium channels. High homocysteine concentration also leads to the shortening of the action potential, loss of the rate adaptation of the action potential and persistent circulation of the re-entry waves. In a series of experimental studies on mice there was an association found between the homocysteine level and activity of vascular inflammation. Elevation of homocysteine level is an independent factor of the thromboembolic events and AF relapses. Population studies showed, that homocysteine is an independent risk factor for AF. So, homocysteine is an interesting target for up-stream therapy.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






