Etiology, clinical characteristics, and outcome of infective endocarditis: 10-year experience from a tertiary care center in Pakistan
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Accepted: 10 March 2022
Authors
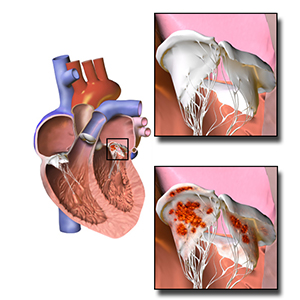
This study was conducted to assess the clinical characteristics, causative agents, complications, and outcomes of infective endocarditis (IE) among patients presenting to our tertiary care center over the last decade. This retrospective cohort study included all adult patients admitted to the Aga Khan University Hospital with the diagnosis of IE over a ten-year period from 2010 to 2020. Outcomes variables included complications during hospitalization, surgical intervention, mortality, and length of stay. We identified a total of 305 cases out of which 176 (58%) were males and 129 (42%) were females. The mean age of the patients was 46.9±18.8 years. 95 (31%) had prosthetic valves in place. Staphylococcus aureus was isolated in 54 (39%) patients followed by coagulase-negative Staphylococcus in 23 (17%). Echocardiography revealed vegetations and abscesses in 236 (77%) and 4 (1%) patients, respectively. The most common valvular complication was mitral valve regurgitation found in 26 (9%) patients, followed by tricuspid valve regurgitation in 13 (4%) patients and aortic valve regurgitation in 11 (3%) patients. Furthermore, 81 (27%) patients suffered from heart failure and 66 (22%) from a stroke during hospitalization. The mean hospital length of stay was 10.4 ± 10.6 days. 64 (21%) patients required surgical repair and the overall mortality rate was 25%. Prosthetic valve endocarditis (OR = 3.74, 95% CI = 2.15-6.50, p<0.001), chronic kidney disease (OR = 2.51, 95% CI = 1.15-5.47, p=0.036), previous stroke (OR = 2.42, 95% CI = 1.18-4.96, p=0.026), and ischemic heart disease (OR = 3.04, 95% CI = 1.50-6.16, p=0.003) were significantly associated with an increased risk of mortality. In conclusion, our study provided valuable data on the clinical characteristics and outcomes of patients with IE in a developing country. S. aureus was the most common causative agent. Heart failure and stroke were the most common complications. The presence of prosthetic valves, history of chronic kidney disease, ischemic heart disease and previous stroke were associated with a significantly increased risk of mortality. Surgical management was not associated with improved outcomes.
Dr. Sohail is a Professor of Medicine at Baylor College of Medicine. He graduated from The Aga Khan University in Pakistan and then pursued Internal Medicine residency at University of Illinois at Chicago-Michael Reese Medical Center, followed by Infectious Diseases fellowship at Mayo Clinic. His research interest is in cardiovascular infections, including cardiovascular implantable electronic device infections, infective endocarditis, ventricular assist device infections, and vascular graft infections. He has published over 180 original peer-reviewed articles in major medical journals. These papers address important clinical questions related to epidemiology, risk factors, clinical presentation, diagnosis, management, complications, outcomes and cost associated with cardiovascular infections. In addition, he has authored 29 book chapters on endocarditis and device infections.
Being an expert in the field of cardiovascular infections, Dr Sohail has been an invited speaker at the meetings of the Heart Rhythm Society, the American Heart Association, the Infectious Diseases Society of America, European Congress of Clinical Microbiology and Infectious Diseases, and the European Society of Cardiology, among others. In addition, he is a Visiting Professor at The Aga Khan University in Karachi, Pakistan.
He is currently a member of the Council of Clinical Cardiology, Council on Quality of Care and Outcomes Research, and Rheumatic Fever, Endocarditis and Kawasaki Disease Committee of the Council on Cardiovascular Disease in the Young for the American Heart Association.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






