Post tuberculosis radiological sequelae in patients treated for pulmonary and pleural tuberculosis at a tertiary center in Pakistan
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
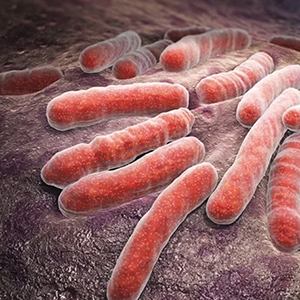
Treating tuberculosis (TB) is not the end of the disease because of the wide spectrum of post TB sequelae associated with the disease. There is insufficient data on post TB radiological sequelae. The aim of this study is to evaluate the post TB radiological sequelae on chest x-rays in patients who had completed the treatment for pulmonary and pleural TB at a tertiary care hospital of a high TB burden country. This is a retrospective cross-sectional study conducted on patients treated for pulmonary and pleural TB. Adult patients (18 years or above) with a clinical or microbiological diagnosis of pulmonary or pleural TB were included. Patients were classified on the basis of site of TB into pulmonary and pleural TB. Post-treatment radiological sequelae on chest x-ray were evaluated and divided into three main types i.e. fibrosis, bronchiectasis and pleural thickening. During the study period a total of 321 patients were included with a mean age of 44(SD±19) years. Only 17.13% (n=55) patients had normal chest x-rays at the end of treatment and 82.87% (n=266) patients had post-TB radiological sequelae with fibrosis being the most common followed by pleural thickening. The post TB radiological sequelae were high in patients who had diabetes mellitus (78.94%), AFB smear-positive (90.19%), AFB culture-positive (89.84%), Xpert MTB/Rif positive (88.40%) and with drug-resistant TB (100%). As a clinician, one should be aware of all the post TB sequelae so that early diagnosis and management can be facilitated.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






