Effects of inhibition of the renin-angiotensin system on hypertension-induced target organ damage: clinical and experimental evidence
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
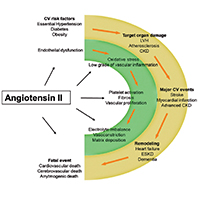
The dysregulation of renin-angiotensin-system (RAS) plays a pivotal role in hypertension and in the development of the related target organ damage (TOD). The main goal of treating hypertension is represented by the long-term reduction of cardiovascular (CV) risk. RAS inhibition either by angiotensin converting enzyme (ACE)-inhibitors or by type 1 Angiotensin II receptors blockers (ARBs), reduce the incidence of CV events in hypertensive patients. Actually, ACE-inhibitors and ARBs have been demonstrated to be effective to prevent, or delay TOD like left ventricular hypertrophy, chronic kidney disease, and atherosclerosis. The beneficial effects of RAS blockers on clinical outcome of hypertensive patients are due to the key role of angiotensin II in the pathogenesis of TOD. In particular, Angiotensin II through an inflammatory-mediated mechanism plays a role in the initiation, progression and vulnerability of atherosclerotic plaque. In addition, Angiotensin II can be considered the hormonal transductor of the pressure overload in cardiac myocytes, and through an autocrine-paracrine mechanism plays a role in the development of left ventricular hypertrophy. Angiotensin II by modulating the redox status and the immune system participates to the development of chronic kidney disease. The RAS blocker should be considered the first therapeutic option in patients with hypertension, even if ACE-inhibitors and ARBs have different impact on CV prevention. ARBs seem to have greater neuro-protective effects, while ACE-inhibitors have greater cardio-protective action.






