Bronchocele, a common but underrecognized condition: a systematic review
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
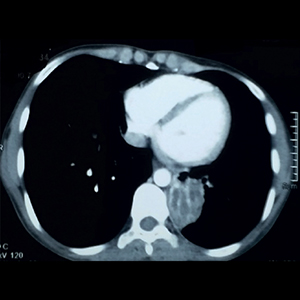
Bronchocele is an abnormal accumulation of mucus often with associated bronchial dilatation. It can be due to either increased production or impaired drainage of mucus in the airways. Diseases like chronic bronchitis, bronchial asthma, bronchiectasis are characterized by high mucus production and other atypical conditions are bronchorrhea and plastic bronchitis with different physical characteristics and compositions of mucus. Improper drainage can lead to bronchocele formation due to underlying benign, malignant tumours or bronchial stenosis. Allergic bronchopulmonary aspergillosis (ABPA) has a peculiar appearance with high attenuated mucus (HAM) in imaging. Careful evaluation of bronchocele is needed as it can be associated with bronchial obstruction or rare causes like plastic bronchitis. Proper identification, evaluation for the underlying cause is key for not missing the underlying diagnosis and accurate treatment.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






