Systemic inflammation in patients with Takotsubo syndrome: a review of mechanistic and clinical implications
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
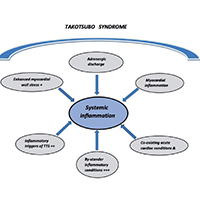
Over recent decades, systemic inflammation as quantified with inflammation markers or indices has been extensively investigated in the setting of various cardiovascular conditions including heart failure (HF), acute coronary syndromes (ACS). In contrast, systemic inflammation in patients with takotsubo syndrome (TTS) has been an underrated phenomenon in clinical practice. On the other hand, experimental and clinical data have been rapidly accumulating in the recent years regarding pathogenetic, prognostic as well as therapeutic implications of systemic inflammation in TTS. Accordingly, the present article aims to provide a general perspective on mechanistic and clinical aspects of systemic inflammation in the setting of TTS.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






