Active cancer and cardiac surgery: Possible scenarios in patient decision-making
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
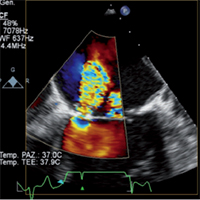
Heart disease and cancer are often found simultaneously in the same patient, and may require cardiac and non-cardiac surgery. Cancer may be part of the past medical history; in other cases the presence of an active malignancy makes the clinical management more complex. No general evidence-based recommendations are available to help in the decision-making process. Because of the lack of specific guidelines we provided a series of possible scenarios describing not unusual cases. We focused on cases where the concomitant presence of heart disease and active malignancies involved a multidisciplinary team. Four real patients with active cancer referred to our Center were assessed. Three of them had valve disease requiring cardiac surgery. Defining the timing of surgery and choosing the surgical approach required a careful and comprehensive evaluation. In the last case, the complicated balance between the thrombotic and the hemorrhagic risk involved difficult decision. Several critical points, which characterized the management of this kind of patients, were identified. In particular, the hemodynamic status, the type and stage of the tumor, the need for cancer therapy, as well as the comorbidities of the patient, had to be taken into account. This narrative review shows the importance of submitting every challenging case to the assessment of a multidisciplinary team, which involves different clinical figures, in order to guarantee the most comprehensive evaluation. When clinical management deviates from the general recommendations, an individualized approach should be used.






